
Peripheral Arterial Disease (PAD) is a commonly occurring disease that involves poor blood circulation from the heart to the body’s extremities, primarily the legs. While it can cause pain and discomfort, PAD can often persist undetected, increasing your risk of heart disease and other major health problems.
In recent years, there has been a sharp increase in the incidence of the most severe forms of PAD – critical limb ischemia or chronic limb-threatening ischemia (CLI/CLTI) – primarily due to rising rates of obesity, diabetes and chronic kidney disease. This is why it is important for patients experiencing symptoms (or those at high-risk for developing PAD) to be screened by a vascular specialist as early as possible.
Treatment for PAD includes diet and exercise, quitting smoking, if applicable, medications and/or minimally invasive surgical procedures.
What Is PAD?
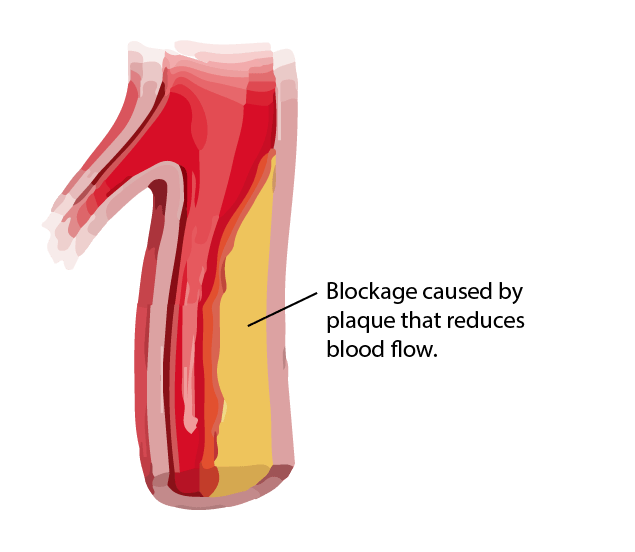
PAD is a serious disorder resulting from the narrowing or blockage of the arteries that carry blood from the heart to the legs, ankles, and feet.
What Causes PAD?
PAD is most commonly caused by atherosclerosis, a disease in which plaque (the buildup of fat, cholesterol, cellular waste, calcium and fibrin) develops on the inner walls of the arteries, causing them to narrow and harden. Narrowing of the arteries causes a decrease of blood flow from the heart to the body’s extremities. If the plaque ruptures, a blood clot may form that narrows the artery even further.
If this process continues unabated, the blood flow becomes so restricted that the organs and tissues below the site of the artery blockage can’t get enough oxygen and nutrients to flourish. Slowly they begin to injure and without the ability to heal, the tissue begins to die (in what’s called gangrene).
What Are the Risk Factors for PAD?
The following conditions and activities may put you at an advanced risk of developing PAD:
- Sedentary lifestyle. Regular physical activity can significantly reduce the risk for developing PAD.
- Smoking. Cigarette smoking not only narrows blood vessels, but it also raises cholesterol levels and blood pressure. Smokers have three times the risk of PAD than nonsmokers.
- Diabetes (type 1 and 2). Diabetes effects such as increased blood clotting, reduced flexibility of blood vessels, and insulin resistance all increase the likelihood of developing PAD.
- Obesity. Obesity increases your risk of several often-interrelated medical problems, including PAD, possibly due to the resulting inflammation clogging your arteries and hindering healing.
- High blood pressure and/or high cholesterol. High blood pressure can harm your arteries increasing your risk of PAD. High cholesterol contributes to the build-up of plaque in the arteries (atherosclerosis), which can significantly reduce the blood’s flow.
- Increasing age. Being over the age of 50, especially 65 and up, increases your chances of developing PAD. Because PAD is a progressive condition, the odds that arterial plaque has built up increase over time, as atherosclerosis generally does not reverse on its own.
- Family history. Either due to genetics or shared poor lifestyle habits, having immediate family members with PAD makes you more likely to also develop it.
How Common Is PAD?
Approximately 6.5 million people over the age of 40 suffer from PAD. However, due to low awareness of PAD and its poor rate of detection the actual number is believed to be significantly higher.
As context, the National Heart, Lung, and Blood Institute at the National Institutes of Health (NIH) states that about half of Americans ages 45 to 84 have atherosclerosis without knowing it. This amounts to roughly 65 million people with the number one cause of PAD.
What Are the Different Stages of PAD?
According to what’s known as the Fontaine Classification system, the stages of PAD are as follows:
- Stage I: Asymptomatic (without symptoms). Patients are mostly asymptomatic, but careful history may reveal subtle and non-specific symptoms such as paresthesias (burning or prickling sensation). Physical examination may reveal cold extremities and other signs of “subclinical” PAD.
- Stage IIa: Intermittent claudication. Patients experience leg pain or discomfort after more than 200 meters of walking.
- Stage IIb: Intermittent claudication. Patients experience leg pain or discomfort after less than 200 meters of walking.
- Stage III: Rest pain. Patients experience pain while at rest, especially at night.
- Stage IV: Ulcers or gangrene. Patients have ischemic ulcers or gangrene.
What Are the Symptoms of PAD?
Many people with PAD may not present with any symptoms, while others may have mild symptoms.
Some of the symptoms noted during PAD include:
- Fatigue in legs when active.
- Pain or cramping that disrupts sleep and is alleviated by lowering feet.
- Lower temperature and sensations in affected leg or foot.
- Suspicious sores including calluses, blisters, or non-healing wounds.
- Poor growth of nails or hair on legs and feet.
- Changes in skin texture (dry or shiny) or color (bluish).
- Muscle weakness or possibly paralysis of affected limb.
Discover more symptoms of PAD.
Does PAD Always Present Symptoms?
PAD often goes undiagnosed because it either advances without showing symptoms, or the symptoms are mistaken for something else.
PAD researchers have also theorized that the up-to-50% of people with PAD who have been found to be “asymptomatic” (i.e. free from leg pain during and after a 6-minute walk test) may simply be restricting their physical activity to avoid painful symptoms.
Do I Need to Get PAD Treated?
It is critical for PAD to be treated as soon as possible. If left untreated, PAD can result in critical limb ischemia (CLI), which can cause constant leg pain, the need for amputation, or even lead to death.
When Should I Visit a Doctor?
If you experience any PAD symptoms, you should see a doctor immediately.
If you are not experiencing symptoms but fall into a high-risk group due to your age (65+) or poor health status (diabetes, smoking history, high cholesterol, high blood pressure) you should be seen by a doctor to screen for PAD. Early diagnosis and intervention is critical.
Why Is Detection of PAD Poor?
PAD’s poor detection rates are the result of a combination of factors. One factor is the nature of the disease, namely its ability to set in slowly, without warning signs that may go unrecognized or falsely attributed. A second (and larger) factor is a lack of awareness among the public of PAD and its dangers. Compared to other health risks such as cancer, PAD does not receive much public attention and surveys have shown that millions of Americans at risk for PAD have never even heard of it.
What Are the Complications of PAD?
Complications of PAD can include:
- Restricted mobility due to pain or discomfort
- Difficulty sleeping
- Difficulty staying warm in cold weather
- Erectile dysfunction in men
- Severe pain in affected extremity especially during rest or inactivity
- Emotional exhaustion from living with chronic disease
- Worsened symptoms when taking cold/allergy medicine with pseudoephedrine
- Death of tissues or gangrene due to infection of open sores
- Amputation (loss of a limb)
- Increased risk of stroke and heart attack
How Is PAD Diagnosed?
PAD diagnosis begins with a medical history review and physical examination, then confirmed through additional, non-invasive testing.
Tests include:
- Ankle brachial index (ABI) test: ABI is a simple test that compares the blood pressure in the upper and lower limbs to determine if there is a discrepancy.
- Arterial duplex ultrasound: ADU is an imaging procedure used to see the arteries in the arms and legs. It can evaluate blood flow and detect any obstructions or blockages.
- Toe brachial index (TBI), also called photoplethysmography (PPG): TBI/PPG uses an infrared light sensor to compare blood pressure in the arms with blood pressure in the toes.
- Computed tomography angiography (CTA): CTA combines a CT scan with an injection of dye to provide images of narrowed blood vessels or blood clots.
- Magnetic Resonance Imaging (MRI): MRI is a non-invasive test that delivers 3D images of blood vessels without the need for contrast dye.
How Is PAD Treated?
Lifestyle Changes and Medication
Treatment begins with lifestyle changes including ceasing smoking, exercising, and reducing alcohol intake. Medications for cholesterol, blood pressure, vasodilators and/or antiplatelets may also be recommended.
Endovascular Solutions
If symptoms are not alleviated by the above, then medical intervention may be required to re-establish blood flow and minimize tissue loss.
This is a minimally invasive process that includes one or up to three of the following:
- Atherectomy: A procedure performed to remove or “debulk” the atherosclerotic plaque from diseased arteries. There are three methods of atherectomy that may be utilized including directional atherectomy, laser atheroablation, or orbital atherectomy. After the atherectomy, an angioplasty may be performed.
- Angioplasty: A balloon is inflated in the narrowed section of the artery to open blockage and restore blood flow. If the angioplasty is not sufficient then a stent may be deployed.
- Stent placement: A stent (small, expandable, mesh-like tube) is placed into the artery to help keep it opened.
Can PAD Be Reversed?
No treatment exists to reverse PAD, but it can be treated to improve symptoms and prevent the condition from progressing. Lifestyle changes, exercise, diet (including a “reversal diet,”) and medication can slow the progression of PAD and help alleviate symptoms.
Conversely, failing to change your lifestyle habits increases your risk of recurring PAD symptoms even after medical treatment.
What Is the Outlook for Someone with PAD?
The outlook for people with PAD depends on their underlying risk factors, the severity of the condition, and the location of the narrowed or blocked artery, among other factors.
There is a high degree of overlap between PAD and coronary artery disease (CAD), and the extent of underlying CAD has a significant impact on the prognosis of patients with PAD.
According to the American College of Cardiology, patients with an ABI of 0.81-0.90 have a two-fold increase in mortality, and those with an ABI ≤0.70 have a four-fold increase in mortality, compared to patients with a normal ABI.
Diagnosing PAD as soon as possible is critically important to future outcomes, because although PAD increases the risk of heart disease, stroke, abdominal aortic aneurysm, amputation, and death, it can often be managed with medication or even simply lifestyle changes.
How Can I Reduce the Risk of Developing PAD?
There are lifestyle changes that can not only reduce the risk of developing PAD but also can slow the progression of the disease. These include:
- Quitting smoking: Stopping smoking can help slow the progression of PAD and have other health benefits, as well.
- Regular exercise: Regular exercise is not only a treatment for PAD, it can help prevent it. It’s much easier to begin a walking program now before PAD makes it painful to walk.
- Healthy weight and diet: Low-cholesterol diet of fruits, vegetables, whole grains, and clean meats.
- Controlled blood sugar, cholesterol, and blood sugar levels.
VasCare Knows PAD & How to Beat It
At VasCare, we treat PAD with the most minimally invasive methods possible to minimize your recovery time and get you back on the road to health as quickly as possible.